Is there a relationship between androgenetic alopecia and COVID-19?
We are currently in the midst of a pandemic situation orchestrated by the SARS-CoV2 (COVID-19) virus. The name SARS stands for Severe Acute Respiratory Syndrome and CoV2 indicates that the virus belongs to the family of Coronaviridae. Coronaviruses are characterized for having a surface covered with protrusions called spikes, giving them a crown-like appearance. Genomic sequence analysis suggest that the virus originated through natural selection in bats or Malayan pangolins and then jumped into humans, a process called “zoonotic transfer” [Lam et al., 2020].
Early epidemiologic reports have shown a disproportionate prevalence of COVID-19 severe cases between adult women and men (42% in males vs 58% in females) [Shi et al., 2020]. Furthermore, a bigger difference is observed in the number of severe COVID-19 cases between pre-pubescent children and adults [Lu et al., 2020]. In children, only 0.6% of COVID-19 cases are severe. In Mexico epidemiological reports are updated daily by Secretaria de Salud. Interestingly, as of July 22, 2020 only 34.8% of COVID-19 deaths were of women whereas 65.18% were men [https://coronavirus.gob.mx/]. An explanation for the skewed prevalence of severe COVID-19 cases between males and females is still unknown.
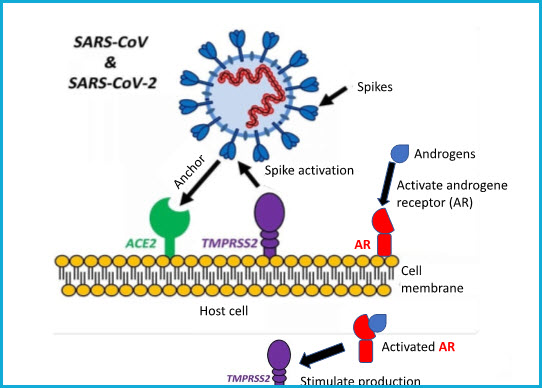
SARS-CoV-2 virus uses its spikes to target and anchor cells to infect. The main virus’ entry point in a host cell is a protein called ACE2. ACE2 is found on the surface of cells from a variety of human organs such as lungs, arteries, heart, kidneys, and intestines. Spikes need to be activated, process known as “priming”, for anchoring host cells. Spike activation is performed by the TMPRSS2 protein, also found on the surface of host cells [Hoffman et al., 2020]. Interestingly, when the androgenetic receptor (AR) is activated, it stimulates the production of TMPRSS2 protein which in turn activates more SARS-CoV2 spikes. Similarly, as in hair follicles, the androgenetic receptor (AR) requires of hormones called androgens (e.g. testosterone) to become activated. The next figure depicts the SARS-CoV2 molecular infection mechanism when encountered with a host cell.
In a study performed between March 23 and April 12, 2020 in three hospitals of Madrid, Spain, dermatologists classified 175 COVID-19 patients as “no alopecia”, “moderate androgenetic alopecia”, or “severe androgenetic alopecia” prior to hospitalization. Results demonstrate that 67% of the patients depict symptoms of moderate or severe androgenetic alopecia. Additionally, 79% of COVID-19 severe cases had androgenetic alopecia as well [Wambier et al., 2020]. These numbers show a clear trend; however, further epidemiological studies are required to assess a correlation between the degree of androgenetic alopecia and the severity of COVID-19 infection. It is worth mentioning that clinical trials highlighting the use of anti-androgen drugs are currently ongoing. These drugs aim at reducing androgen levels, thus decreasing the activation of androgenetic receptors in COVID-19 patients.
All these observations have led scientists to study the potential correlation between androgenetic alopecia with the severity of COVID-19 infection under the hypothesis that places androgens as the main cause of COVID-19 severity. The potential correlation between androgenetic alopecia and COVID-19 has been termed the “Gabrin Sign” in honor of Doctor Frank Gabrin, the first American physician who died of COVID-19 [Wambier et al., 2020]. Interestingly, Doctor Gabrin suffered from androgenetic alopecia and was victim of a severe COVID-19 infection.
At CapilarFix® we are not experts in COVID-19 however we are skilled in treating alopecia. Perhaps (we can’t be sure yet), by treating androgenetic alopecia we could indirectly be lowering the risk of severe COVID-19 infection.
References:
Lam, T.T., Jia, N., Zhang, Y. et al. Identifying SARS-CoV-2-related coronaviruses in Malayan pangolins. Nature 583, 282–285 (2020). https://doi.org/10.1038/s41586-020-2169-0
Shi Y., Yu X., Zhao H., Wang H., Zhao R., Sheng J. Host susceptibility to severe COVID-19 and establishment of a host risk score: findings of 487 cases outside Wuhan. Crit Care. 2020;24(1):108.
Lu X, Zhang L, Du H, et al. SARS‐CoV‐2 infection in children. N Engl J Med. 2020.
Hoffmann M., Kleine-Weber H., Schroeder S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020:1–10.
Wambier, C. G., Vaño-Galván, S., McCoy, J., Gomez-Zubiaur, A., Herrera, S., Hermosa-Gelbard, Á., Moreno-Arrones, O. M., Jiménez-Gómez, N., González-Cantero, A., Fonda-Pascual, P., Segurado-Miravalles, G., Shapiro, J., Pérez-García, B., & Goren, A. (2020). Androgenetic alopecia present in the majority of patients hospitalized with COVID-19: The “Gabrin sign”. Journal of the American Academy of Dermatology, 83(2), 680–682. https://doi.org/10.1016/j.jaad.2020.05.079